Those with low incomes in the United States are primarily covered by Medicaid, the public health insurance programme.
Medicaid in some states will pay for routine checkups and corrective lenses, while in others it will only pay for emergencies. Adult vision services are another form of optional coverage that states can choose to offer or not.
From 2001-2008, Medicaid adult vision benefits were offered in 29-33 states.
Our findings indicate that a rise of up to 10% in the proportion of Medicaid beneficiaries with properly corrected distance vision is linked to Medicaid’s coverage of adult vision care.
Keep reading to know more on Vision Medicaid!
Read Also:
List of Eye doctors that accept Medicaid near me, check here.
Does Medicaid Cover Glasses? Check glasses coverage by medicaid.
Does Medicaid Cover Vision?
Medicare’s decision to cover eye care depends on both the patient’s age and the underlying medical condition.
The availability of Medicaid services varies from one U.S. state to the next. U.S. citizens and legal permanent residents under the age of 21 who are enrolled in an EPSDT (Early, Periodic Screening, Diagnostic, and Treatment) programme are eligible for Medicaid coverage of vision care.
Vision care, including testing and treatment, is covered by Medicaid.
It gets more complicated once a person reaches the age of 21, as each state has the power to decide whether or not Medicaid will cover their vision care.
Medicaid will only pay for appointive eye surgery if it is considered medically necessary.
Does Medicaid Cover Vision For Adults
The state’s Medicaid programme covers limited vision care services for adults. These services are as following :
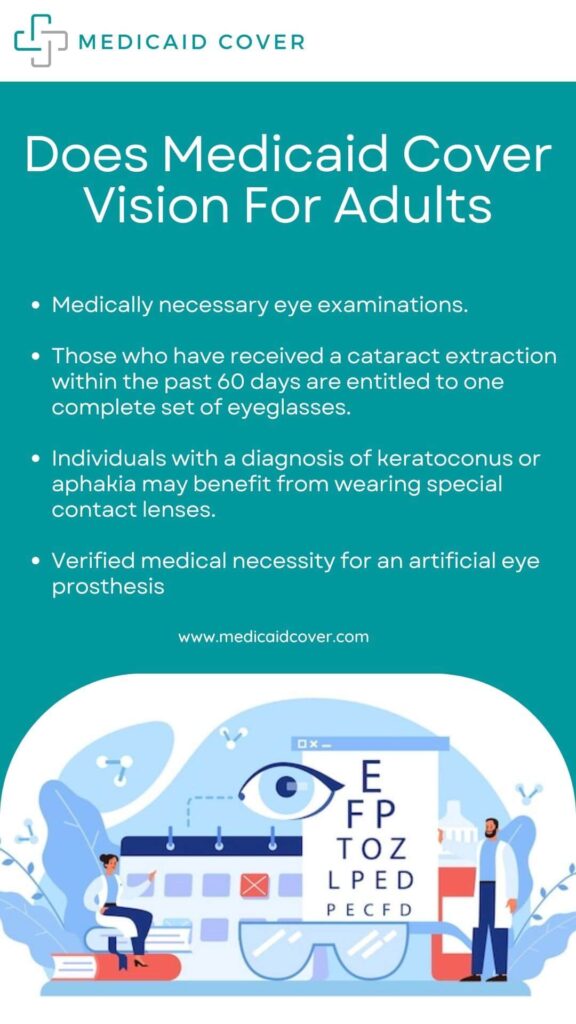
- Medically necessary eye examinations.
- Those who have received a cataract extraction within the past 60 days are entitled to one complete set of eyeglasses.
- Individuals with a diagnosis of keratoconus or aphakia may benefit from wearing special contact lenses.
- Verified medical necessity for an artificial eye prosthesis
Does Medicaid Cover Vision Care For Children
One out of every four children has a vision problem. 2 These problems, alas, are not distributed uniformly. A child’s risk of visual impairment is nearly doubled if they are from a low-income family compared to a family with a higher income.
In order to provide comprehensive and preventative health care services, Medicaid offers the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) benefit to Medicaid enrollees with children younger than 21 years old.
The following are some of the ways in which EPSDT can be useful : –
- Identifying health issues early
- Scheduling routine checkups for kids (based on age)
- Giving people the opportunity to have their health, mental state, development, dental, hearing, and eyesight checked to identify issues
- As soon as a potential threat is identified, diagnostic tests are performed.
- Correct, mitigate, or eliminate health issues by receiving appropriate care.
Medicaid is a valuable tool that can help a lot of kids get the eye care they need. However, many households initially require assistance in order to overcome substantial obstacles.
Does Medicaid Cover Vision Therapy?
The answer to whether or not Medicaid covers vision care depends on the patient’s age, the state in which they reside, and the reason for the care.
For children under the age of 21, Medicaid’s Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) programme covers all necessary eye care costs.
However, things become less clear for adults over the age of 21, as each state makes its own decisions regarding whether and how often to cover vision care (including exams, eyeglasses, contact lenses, and therapy).
Here, the rules are determined by the health insurance provision.
Vision Care Coverage With Medicaid
Additional screenings and diagnostics should be performed if a problem is suspected. Medicaid does not cover the cost of routine checkups for children. The Children’s Health Insurance Program provides this coverage (CHIP)
Although federal guidelines do not mandate it, some states will also make these services available to adult Medicaid beneficiaries.
Coverage for adult vision care under Medicaid can vary by state, but may include glaucoma screenings, cataract surgeries, other medical and surgical procedures, contact lenses, eyeglasses, and even reduced copays.
Types Of Vision Care Providers
Ophthalmologists, optometrists, and opticians are the three primary specialists in the field of eye care.
Examining and treating eye diseases is a specialty shared by ophthalmologists and optometrists.
-
An Ophthalmologist
When it comes to the health of one’s eyes and vision, he is the man to see.
An M.D. or D.O. (Doctor of Osteopathy) degree is required for entry into the field of ophthalmology after completion of undergraduate studies.
The residency programme for an eye M.D. is designed to give the resident extensive training in all aspects of eye care, from prevention and diagnosis to medical and surgical treatment.
-
An Optometrist
He holds the prestigious O.D. (Doctor of Optometry) designation (not to be confused with a Doctor of Medicine, an M.D.). Professional optometry training consists of a 4-year programme after 4 years of undergraduate study in a pre-professional field.
Low vision rehabilitation, primary eye care, geriatric optometry, pediatric optometry, family eye care, contacts, sports vision, and vision therapy are just some of the subspecialties that some optometrists pursue after completing their general optometry residency.
-
Opticians
They know how to take a prescription for eyewear and fill it, as well as how to pick out the best frames and make any necessary adjustments so the glasses fit perfectly.
The fitting of contact lenses is a specialty that may require certification in some states. Opticians may work alongside other eye care professionals, such as optometrists and ophthalmologists, or they may operate their own business.
Eligibility For Medicaid Vision Coverage
Medicaid, which covers medical expenses for low-income people, insures and treats more than 70 million Americans. Medicaid coverage is mandated by law for the following in the United States:
- Families with low incomes, defined as those earning 135 percent or less of the federal poverty line (FPL)
- Eligible infants and mothers
- People who have physical impairments, such as blindness
- Those who are eligible for Supplemental Security Income (SSI)
Medicaid is a federal programme, but each state has its own version, and eligibility requirements and benefits can be modified to cover more people, such as low-income adults. Regular checkups provided by Medicaid should include vision screenings as part of preventative care.
Routine vision exams can detect any problems that may arise. After that, you can be referred to specialists for further testing.
These vision services are required to be provided to all Medicaid enrollees by federal regulations, but individual states have the authority to decide whether or not to cover vision costs for adults. Your doctor will be the best person to advise you on what medical care is covered and how much it will cost.
How To Take Advantage Of Your Medicaid Vision Benefits?
Medicaid patients who are eligible for vision care must typically obtain a referral from their primary care physician before seeing a specialist.
Visit Benefits.gov to find contact information for your regional Medicaid office. Here you can locate a Medicaid center near you by selecting the appropriate State and then selecting the appropriate subcategory (Medicaid).
Here you can locate a Medicaid center near you by selecting the appropriate State and then selecting the appropriate subcategory (Medicaid).
Your eye doctor is another resource for learning how to maximize your Medicaid vision coverage.
Some doctors won’t take Medicaid, but they can direct you to facilities that do.
What Vision Benefits Medicaid Cover In Every State?
There are two categories of visual benefits :-
-
Mandatory Medicaid Vision Benefits
As a matter of federal law, all US state Medicaid programs must cover specific eye care services. This includes certain types of eye care, such as exams and surgery, for which Medicaid will pay in full under certain circumstances.
-
Optional Medicaid Vision Benefits
When it comes to vision care, Medicaid will pay for services that aren’t strictly necessary but are still beneficial to the patient. The Medicaid coverage for services like optometry and eyewear varies by state.
When Medicaid Cover Eye Surgery?
In order for Medicaid to pay for cataract surgery, it must be deemed “medically necessary.” The removal of cataracts and other surgical procedures on the eyes may fall under this category.
Medicaid will occasionally pay for cosmetic eye surgery. Diseases and injuries that impair your eyesight may be covered by medical insurance, and an ophthalmologist can help.
If two conditions are met, then Medicaid will cover the cost of the elective surgery.
- It’s the cheapest possible treatment option
- There is a valid medical justification for this.
Necessary Procedures
Medically necessary eye surgeries performed by an ophthalmologist are likely to be covered by Medicaid under the health insurance module, which means standard guidelines for these procedures are being applied consistently across the country.
- Diseases like diabetes, gout, keratoconus, multiple sclerosis, and others can be avoided or have their symptoms alleviated through surgical intervention.
- Surgical treatment for problems with the eye, including the iris, pupil, sclera, retina, optic nerve, cornea, conjunctiva, lids, and more.
Lasik
Medicaid almost never covers refractive surgery like LASIK because cheaper and less invasive options like glasses and contacts already exist.
Due to the availability of less expensive methods of correcting vision, Laser In-Situ Keratomileusis (LASIK) is never required for medical purposes. This also applies to corrective eye surgery for refractive errors rather than for medical conditions.
- Radial Keratotomy (RK)
- Laser Epithelial Keratomileusis (LASEK)
- Photorefractive Keratectomy (PRK)
- Epipolar Laser In Situ Keratomileusis (Epi-LASIK)
- Refractive Lens Exchange (RLE)
Cataract
Cataract surgery is more likely to be covered by Medicaid when the lens has become cloudy and significantly impairs vision. If the cataract is causing you significant visual impairment, your plan administrator may consider the procedure medically necessary.
The eye doctor will remove the damaged lens and replace it with a synthetic one. However, the majority of the high-end choices for a cataract replacement lens are ruled out by the least expensive alternative rule.
- The most cost-effective intraocular lenses are mono focal designs.
- There is usually no budget for fancier add-ons
- In exceptional cases, medicaid may cover:
-
- PanOptix trifocal lens
- Toric lenses (astigmatism-correcting)
- Symfony EDOF (extended-depth-of-focus)
Does Medicaid Pay For Vision Exams?
When it comes to eye exams, many clinics will accept Medicaid patients as long as they fall within the guidelines set forth by the programme.
If, for example, your state only pays for one eye exam every three years and you schedule an appointment after two years, the second exam will not be covered. But there are some exceptions, like if you have a preexisting condition that necessitates more frequent checkups.
Frequently Asked Questions
How much does Medicaid cover for vision?
Copayments for eye exams vary from free in some states to $15 in others. Most states also have separate copayment structures for minors and adults.
Insurance for glasses may be included in your plan or offered as an optional add-on in your state of residence. Know what is and is not covered by Medicaid in regards to vision care by checking the requirements of your state’s programme.
What does Medicaid cover for vision?
Eligible Medicaid recipients typically receive protection from financial hardship by having the following costs covered:
- Providing medical care
- Prenatal and postnatal care
- Diagnostic imaging and laboratory services
- Medical services for the general public at select hospitals
- Patient admissions and discharges (excluding institutions for mental illness)
- In-Home Medical Care and Other Services
- Individuals under the age of 21 are encouraged to take advantage of free health screenings.
- Vision insurance (coverage varies by state).
How bad does my vision need to be for priority health Medicaid to cover glasses?
Is there anything to do if you’re worried about vision loss, eye pain, or other symptoms that could indicate a serious problem with your eyes? You should visit an ophthalmologist if you have glaucoma, cataracts, or any other serious eye condition. An ophthalmologist is a doctor who focuses on treating eye and vision problems.
Ophthalmologists are medical doctors who specialize in the diagnosis and treatment of diseases of the eye as well as in the surgical and medical correction of vision (including the prescription of glasses and contact lenses).
Conclusion : –
Medicaid recipients who also qualify for vision care have a much better chance of receiving corrective lenses for their distance vision. It may be necessary to conduct additional studies on the effects of Medicaid coverage on other services, as well as the effects of vision coverage on related functional outcomes.